Researchers from The University of Texas Health Science Center at San Antonio (UT Health San Antonio) have discovered that a metabolite found in urine predicts kidney failure from type 2 diabetes five to 10 years early. This new research, published in the Journal of Clinical Investigation, showed that adenine, a metabolite produced in the kidney was both a predictive and causative biomarker of progressive kidney disease.
The new finding has the potential to upend the current method of detecting advancing kidney disease which focuses on the presence of the protein albumin in the urine, as data from the UT Health San Antonio investigators show nearly half of the patients with progressive kidney disease do not show significant protein levels in their urine. This produces a significant diagnostic gap as the team notes roughly 90% of all diabetes patients with low albumin levels remains at risk of kidney failure. Using albumin as a biomarker of kidney disease risk has the potential to get more at-risk patients on treatment programs years in advance before kidney failure manifests, noted the study’s senior author, Kumar Sharma, MD, professor and chief of nephrology at UT Health San Antonio. Kumar is also the founding director of the health system’s Center for Precision Medicine.
In addition to diagnostic potential of adenine as a more robust predictor of kidney failure risk, the team also identified a small molecule that blocks the major pathway of endogenous adenine production in the body. Using a mouse model of type 2 diabetes, the researchers showed drug reduced adenine levels in the animals.
“The drug protected against all the major aspects of diabetic kidney disease without affecting blood sugar,” Sharma said. “The study is remarkable as it could pave the way to precision medicine for diabetic kidney disease at an early stage of the disease.”
For their work, the investigators used data from three international cohorts of patients comprising 1,200 patients from diverse populations that included African American, Hispanic, Caucasian, American, and Asian groups. A consistent pattern across all cohorts showed a consistently strong association between elevated urine adenine levels and a higher risk of kidney failure.
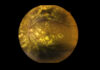
To better understand the spatial distribution of adenine and other small molecules in kidney tissues, the team applied spatial metabolomics on kidney biopsies from human patients, which allowed them to pinpoint the locations of adenine within kidney tissue. “It’s a very difficult technique, and it took us several years to develop a method where we combine high resolution of the geography of the kidney with mass spectrometry analysis to look at the metabolites,” Sharma noted.
Findings from this analysis showed endogenous adenine around scarred blood vessels in the kidney and around tubular-shaped kidney cells that were being destroyed. Interestingly, the research also showed that elevated levels of adenine was also associated with all-cause mortality, which suggests the metabolite may be affecting other areas of the body.
But when it comes to kidney failure that is driven by the development of diabetes, the need for new diagnostic modalities and early treatments is clear. Once a patient is identified with kidney disease the treatment regimen is to receive kidney dialysis three times a week to help clean their blood. Patients on dialysis with kidney failure from diabetes have a 40% mortality rate within five years.
While treatments are improving, they are only advancing in small increments—patients still have progressive kidney disease and kidney failure, but they have a bit more time before reaching the endpoint.
“What we’re hoping is that by identifying patients early in their course and with new therapies targeting adenine and kidney scarring, we can block kidney disease or extend the life of the kidney much longer,” Sharma concluded.